Stereotaxy-guided lesionectomy with oncological criteria in a patient with epileptic seizures
DOI:
https://doi.org/10.59156/revista.v39i02.759Keywords:
Epileptic Seizures, Gangliogliomas, Gliomas, Stereotactic GuidanceAbstract
Background: in patients with epileptic seizures and suspected glial lesions, whether low- or high-grade, the surgical approach is primarily defined by oncological criteria. In the case of low-grade gliomas, complete resection is associated with a significant improvement in overall survival. However, some of these lesions may be small and located in deep regions of the brain, which represents a technical challenge. In these cases, the use of tools such as neuronavigation or stereotaxy allows for precise and safe localization of the lesion, thus optimizing surgical planning and reducing the risk of neurological sequelae.
Objectives: to describe a case of stereotaxy-guided lesionectomy with oncological criteria in a patient with epileptic seizures.
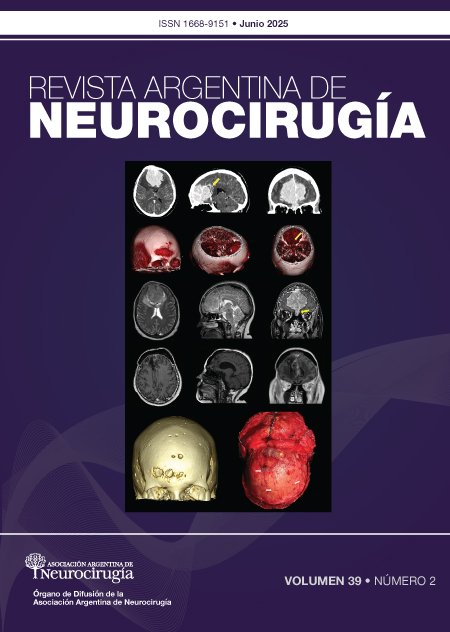
Case description: a 28-year-old female patient with no significant medical history presented with absence seizures, holocranial headache, nausea, and vomiting of three years' duration. Magnetic resonance imaging with spectroscopy revealed a lesion in the right temporal lobe characterized by an increased choline peak and a decreased N-acetyl aspartate level, findings preliminarily consistent with a primary tumor. The electroencephalogram showed slow background activity in the right centrotemporal region. Given this combination of clinical, radiological, and electrophysiological findings, it was decided to perform oncological surgery, prioritizing this approach over a purely epileptogenic approach.
Surgery: a stereotactic-guided lesionectomy was performed via a right temporal approach, using a caudal-based horseshoe incision. A craniotomy was performed centered over the path of the stereotactic needle, followed by an inferior-based "C" dural opening and a minimal corticotomy following this path until the lesion was located. Complete resection was achieved. The patient had a favorable postoperative course and was discharged from the hospital on the sixth day. The pathological study confirmed the diagnosis of ganglioglioma, grade I according to the WHO classification.
Conclusions: when a patient with epileptic seizures presents with a suspected glial lesion, the surgical approach is oncological, aiming for maximal and safe resection. The use of stereotaxy is effective in locating small and deep lesions. If the patient persists with epileptic seizures, an approach focused on epilepsy surgery is proposed.
Downloads
References
Chang EF, Potts MB, Keles GE, Lamborn KR, Chang SM, Barbaro NM, Berger MS.. Seizure characteristics and control following resection in 332 patients with low-grade gliomas. J Neurosurg, 2008; 108(2): 227-35. Doi: 10.3171/JNS/2008/108/2/0227
Englot DJ, Berger MS, Barbaro NM, Chang EF. Predictors of seizure freedom after resection of supratentorial low-grade gliomas. A review. J Neurosurg, 2011; 115(2): 240-4. https://doi.org/10.3171/2011.3.JNS1153
Englot DJ, Berger MS, Chang EF, Garcia PA. Characteristics and treatment of seizures in patients with high-grade glioma: a review. Neurosurg Clin N Am, 2012; 23(2): 227-35. viii. https://doi.org/10.1016/j.nec.2012.01.009
Gildenberg PL, Woo SY. Multimodality program involving stereotactic surgery in brain tumor management. Stereotact Funct Neurosurg, 2000; 75(2-3): 147-52. Doi:10.1159/000048397.
Rheims S, Ducray F, Ryvlin P. Choosing the tumoral epilepsy surgery candidate. Epilepsia, 2013; 54 Suppl 9: 91-6. Doi:10.1111/epi.12451.
Uribe-Cardenas R, Giantini-Larsen AM, Garton A, Juthani RG, Schwartz TH. Innovations in the diagnosis and surgical management of low-grade gliomas. World Neurosurg, 2022; 166: 321-7. Doi:10.1016/j.wneu.2022.06.070