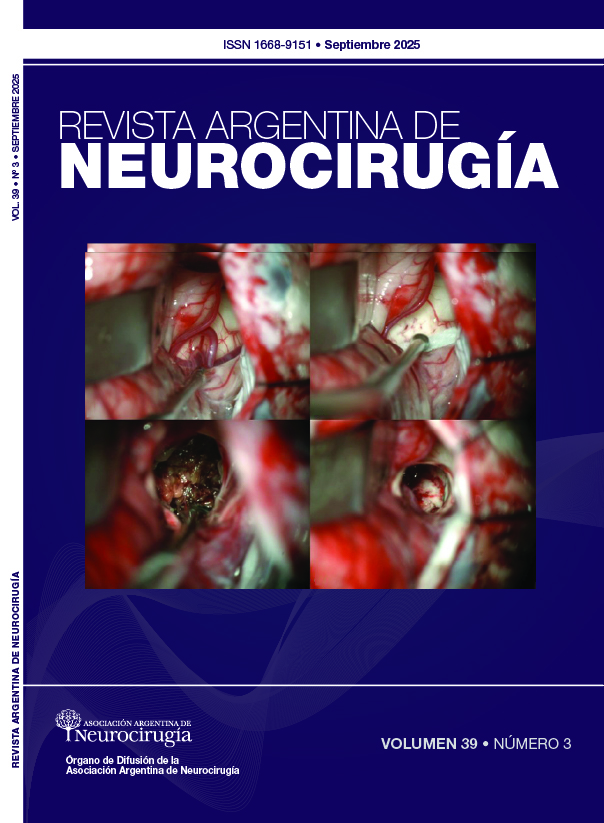
Surgical approach to chronic subdural hematoma: review of pathophysiology and experience at our center
DOI:
https://doi.org/10.59156/t129pj18Keywords:
Chronic subdural hematoma, Subdural drainage, Subdural, Subperiostal drainageAbstract
Background: chronic subdural hematoma (cSDH) is a common neurosurgical entity in older adults, characterized by persistent inflammation of a neomembrane with fragile neovascularization and episodes of recurrent microhemorrhage. Despite standard surgical management using burr hole and subdural drainage, symptomatic recurrence rates remain high, reaching up to 20% in some series.
Objectives: to evaluate clinical efficacy and recurrence rates associated with a subperiosteal drain with a wide subgaleal pocket in patients undergoing surgery for cSDH at a tertiary center.
Methods: this was a retrospective study including 213 adult patients who underwent evacuation of cSDH using burr hole and subperiosteal drainage. Clinical, surgical, and short- and medium-term follow-up variables were analyzed.
Results: the mean age was 69.6 years; 67.4% were men. The most common symptom was motor deficit (73.71%), followed by sensory disturbance (52.58%). A single trephine was used in 81.22% of cases. Drain removal was performed within the first 48 hours in 89.11% of patients. The rate of symptomatic recurrence requiring reintervention was 3.37%, markedly lower than that reported in traditional series with subdural drains.
Conclusions: a subperiosteal drainage with a wide subgaleal pocket showed excellent clinical results: low recurrence rate, rapid recovery, and minimal complications. The technique proved effective even in patients with comorbidities and on anticoagulant therapy.
Downloads
References
1. Edlmann E, Giorgi-Coll S, Whitfield PC, Carpenter KLH, Hutchinson PJ. Pathophysiology of chronic subdural haematoma: inflammation, angiogenesis and implications for pharmacotherapy. J Neuroinflammation. 2017 May 30;14(1):108. doi: 10.1186/s12974-017-0881-y.
2. Kolias AG, Chari A, Santarius T, Hutchinson PJ. Chronic subdural haematoma: modern management and emerging therapies. Nat Rev Neurol. 2014 Oct;10(10):570-8. doi: 10.1038/nrneurol.2014.163.
3. Feghali J, Yang W, Huang J. Updates in chronic subdural hematoma: epidemiology, etiology, pathogenesis, treatment, and outcome. World Neurosurg. 2020 Sep;141:339-45. doi: 10.1016/j.wneu.2020.06.140.
4. Ironside N, Nguyen C, Do Q, Ugiliweneza B, Chen CJ, Sieg EP, James RF, Ding D. Middle meningeal artery embolization for chronic subdural hematoma: a systematic review and meta-analysis. J Neurointerv Surg. 2021 Oct;13(10):951-7. doi: 10.1136/neurintsurg-2021-017352.
5. Macdonald RL. Pathophysiology of Chronic Subdural Hematomas. En: Youmans and Winn Neurological Surgery, 46, 353-9.e2
6. Chari A, Kolias AG, Borg N, Hutchinson PJ, Santarius T. Medical and surgical management of chronic subdural hematomas. En: Youmans and Winn Neurological Surgery, 46, 353-9.e2
7. Nouri A, Gondar R, Schaller K, Meling T. Chronic Subdural Hematoma (cSDH): A review of the current state of the art. Brain Spine. 2021 Nov 2;1:100300. doi: 10.1016/j.bas.2021.100300.
8. Khan I, Shakir M, Hika B, Khan M, Bhatti IA, Qureshi AI, Thomas A, Kan P, Siddiq F. Failure rates of conservative management of minimally symptomatic chronic subdural hematoma: a systematic review and meta-analysis. World Neurosurg. 2024 Nov;191:291-302.e1. doi: 10.1016/j.wneu.2024.09.002.
9. Weigel R, Schmiedek P, Krauss JK. Outcome of contemporary surgery for chronic subdural haematoma: evidence based review. J Neurol Neurosurg Psychiatry. 2003 Jul;74(7):937-43. doi: 10.1136/jnnp.74.7.937.
10. Lega BC, Danish SF, Malhotra NR, Sonnad SS, Stein SC. Choosing the best operation for chronic subdural hematoma: a decision analysis. J Neurosurg. 2010 Sep;113(3):615-21. doi: 10.3171/2009.9.JNS08825.
11. Almenawer SA, Farrokhyar F, Hong C, Alhazzani W, Manoranjan B, Yarascavitch B, Arjmand P, Baronia B, Reddy K, Murty N, Singh S. Chronic subdural hematoma management: a systematic review and meta-analysis of 34,829 patients. Ann Surg. 2014 Mar;259(3):449-57. doi: 10.1097/SLA.0000000000000255.
12. Srivatsan A, Mohanty A, Nascimento FA, Hafeez MU, Srinivasan VM, Thomas A, Chen SR, y col. Middle meningeal artery embolization for chronic subdural hematoma: meta-analysis and systematic review. World Neurosurg. 2019 Feb;122:613-9. doi: 10.1016/j.wneu.2018.11.167.
13. Schmolling ÁH, Pérez-García C, Trejo C, López-Frías A, Jaroenngarmsamer T, Rosati S, y col. Middle meningeal artery embolization for management of chronic subdural hematoma. Radiographics. 2024 Apr;44(4):e230158. doi: 10.1148/rg.230158.
14. Davies JM, Knopman J, Mokin M, Hassan AE, Harbaugh RE, Khalessi A, EMBOLISE Investigators y col. Adjunctive middle meningeal artery embolization for subdural hematoma. N Engl J Med. 2024 Nov 21;391(20):1890-900. doi: 10.1056/NEJMoa2313472.
15. Jensen TSR, Haldrup M, Hjortdal Grønhøj M, Miscov R, Larsen CC, Debrabant B, y col. National randomized clinical trial on subdural drainage time after chronic subdural hematoma evacuation. J Neurosurg. 2021 Dec 31;137(3):799-806. doi: 10.3171/2021.10.JNS211608.
16. Raj R, Tommiska P, Koivisto T, Leinonen V, Danner N, Posti JP, y col. Burr-hole drainage with or without irrigation for chronic subdural haematoma (FINISH): a Finnish, nationwide, parallel-group, multicentre, randomised, controlled, non-inferiority trial. Lancet. 2024 Jun 29;403(10446):2798-806. doi: 10.1016/S0140-6736(24)00686-X.
17. Santarius T, Kirkpatrick PJ, Ganesan D, Chia HL, Jalloh I, Smielewski P, y col. Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: a randomised controlled trial. Lancet. 2009 Sep 26;374(9695):1067-73. doi: 10.1016/S0140-6736(09)61115-6.
18. Nakaguchi H, Tanishima T, Yoshimasu N. Factors in the natural history of chronic subdural hematomas that influence their postoperative recurrence. J Neurosurg. 2001 Aug;95(2):256-62. doi: 10.3171/jns.2001.95.2.0256.
19. Stanišic M, Pripp AH. A reliable grading system for prediction of chronic subdural hematoma recurrence requiring reoperation after initial burr-hole surgery. Neurosurgery. 2017 Nov 1;81(5):752-760. doi: 10.1093/neuros/nyx090.
20. Mack J, Squier W, Eastman JT. Anatomy and development of the meninges: implications for subdural collections and CSF circulation. Pediatr Radiol. 2009 Mar;39(3):200-10. doi: 10.1007/s00247-008-1084-6.
21. Izumihara A, Yamashita K, Murakami T. Acute subdural hematoma requiring surgery in the subacute or chronic stage. Neurol Med Chir (Tokyo). 2013;53(5):323-8. doi: 10.2176/nmc.53.323.
22. Nabeshima S, Reese TS, Landis DM, Brightman MW. Junctions in the meninges and marginal glia. J Comp Neurol. 1975 Nov 15;164(2):127-69. doi: 10.1002/cne.901640202.
23. Moskala M, Goscinski I, Kaluza J, Polak J, Krupa M, Adamek D, y col. Morphological aspects of the traumatic chronic subdural hematoma capsule: SEM studies. Microsc Microanal. 2007 Jun;13(3):211-9. doi: 10.1017/S1431927607070286.
24. Yamashima T, Yamamoto S, Friede RL. The role of endothelial gap junctions in the enlargement of chronic subdural hematomas. J Neurosurg. 1983 Aug;59(2):298-303. doi: 10.3171/jns.1983.59.2.0298
25. Ito H, Yamamoto S, Komai T, Mizukoshi H. Role of local hyperfibrinolysis in the etiology of chronic subdural hematoma. J Neurosurg. 1976 Jul;45(1):26-31. doi: 10.3171/jns.1976.45.1.0026.
26. Hohenstein A, Erber R, Schilling L, Weigel R. Increased mRNA expression of VEGF within the hematoma and imbalance of angiopoietin-1 and -2 mRNA within the neomembranes of chronic subdural hematoma. J Neurotrauma. 2005 May;22(5):518-28. doi: 10.1089/neu.2005.22.518.
27. Hong HJ, Kim YJ, Yi HJ, Ko Y, Oh SJ, Kim JM. Role of angiogenic growth factors and inflammatory cytokine on recurrence of chronic subdural hematoma. Surg Neurol. 2009 Feb;71(2):161-5; discussion 165-6. doi: 10.1016/j.surneu.2008.01.023.