Cerebral cognitive mapping as an alternative for the safe resection of abscessed metastasis secondary to neuroendocrine neoplasm
DOI:
https://doi.org/10.59156/revista.v39i03.739Keywords:
Abscessed metastasis, Cognitive mapping, Neuroendocrine neoplasia, Safe resectionAbstract
Background: abscessed brain metastases are an extremely rare manifestation of oncological pathologies, particularly in patients with neuroendocrine tumors. Their clinical and radiological presentation can mimic pyogenic abscesses or high-grade gliomas, which affects the differential diagnosis and therapeutic options. The choice of an awake surgical technique with intraoperative multimodal cognitive mapping, traditionally reserved for low-grade gliomas, allowed for oncologically safe resection without generating permanent neurological deficits.
Objectives: to describe a case approached using an alternative surgical technique with multimodal cognitive mapping, achieving complete resection without new neurological deficits.
Case description: a 66-year-old female patient presented primarily with episodes of disorientation. Magnetic resonance imaging revealed a mesial temporal lesion with central cystic-like areas with perilesional edema and heterogeneous enhancement. A high-grade glial lesion was suspected.
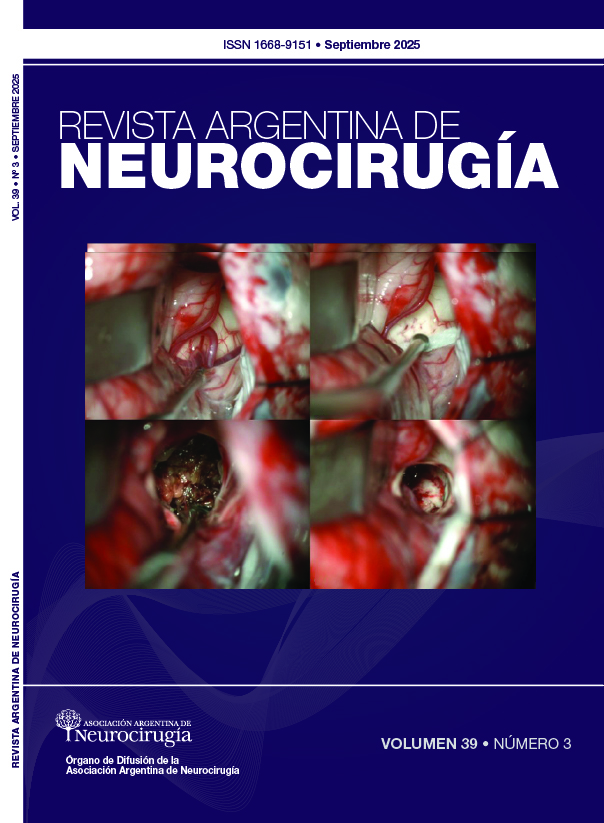
Surgery: an awake craniotomy was performed using intraoperative cortical mapping techniques using direct stimulation and cognitive tasks. Critical functional areas were identified, and a complete resection was achieved. Histopathology confirmed metastasis with inflammatory changes and necrosis suggestive of abscessation. A positive finding on upper gastrointestinal video endoscopy revealed cells suggestive of neuroendocrine cancer.
Conclusion: awake surgery with cognitive mapping allows for a safe approach to metastatic lesions in eloquent regions, even in complex cases with prior cognitive impairment. This approach represents a valuable tool for optimizing the balance between oncological control and functional preservation.
Downloads
References
Nayak L, Lee EQ, Wen PY. Epidemiology of brain metastases. Curr Oncol Rep, 2012; 14(1): 48-54.
Soffietti R, Abacioglu U, Baumert B, et al. Diagnosis and treatment of brain metastases from solid tumors: guidelines from the European Association of Neuro-Oncology (EANO). Lancet Oncol, 2017; 19(2): 162-74.
Küker W, Nägele T, Schmidt F, et al. Diffusion-weighted MRI in brain abscesses and necrotic brain tumors: the role of the apparent diffusion coefficient. Neuroradiology, 2005; 47(10): 651-6.
Shankar JJ, Vandorpe R. Brain abscess mimicking metastasis. Can Assoc Radiol J, 2011; 62(1): 52-3.
Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol, 2008; 26(18): 3063-72.
Patel JK, Didolkar MS, Pickren JW, Moore RH. Metastatic pattern of carcinoid tumors. Cancer, 1974; 33(1): 107-14.
Krug S, Teupe F, Michl P, Gress TM, Rinke A. Brain metastases in patients with neuroendocrine neoplasms: risk factors and outcome. BMC Cancer, 2019; 19(1): 362.
Korse CM, Taal BG, van Velthuysen ML, Visser O. Incidence and survival of neuroendocrine tumors in the Netherlands according to histological grade: experience of all 95 Dutch pathology laboratories. Ann Oncol, 2013; 24(2): 614-8.
Gerritsen JKW, Arends L, Klimek M, Vincent AJPE. Awake craniotomy for brain tumor resection: a systematic review of clinical outcomes and safety in glioblastomas and brain metastases. Acta Neurochir (Wien), 2019; 161(1): 99-106.
Nossek E, Matot I, Shahar T, et al. Intraoperative awake craniotomy for brain tumor resection: the Tel-Aviv Medical Center 10-year experience. J Neurosurg, 2011; 114(6): 1113-8.
De Witt Hamer PC, Berger MS, Chang EF, et al. Impact of awake mapping on glioma surgery outcome: a review and meta-analysis. J Clin Oncol, 2012; 30(20): 2559-65.
Lee CZ, Poon CCM. An update of neuroanesthesia for intraoperative brain mapping craniotomy. Neurosurgery, 2022; 90(1): 1-6.
Szelényi A, Bello L, Duffau H, et al. Intraoperative electrical stimulation in awake craniotomy: methodological aspects of current practice. Neurosurg Focus, 2010; 28(2): E7. doi:10.3171/2009.12.FOCUS09237.
Caplin ME, Baudin E, Ferolla P, et al. Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice. Ann Oncol, 2015; 26(8): 1604-20.
Singh S, Asa SL, Dey C, et al. Diagnosis and management of gastrointestinal neuroendocrine tumors: an evidence-based Canadian consensus. Cancer Treat Rev, 2016; 47: 32-45.